Oral HPV Testing: A New Dental Approach to an Old Problem
Mohammad Kamal, MD
Human Papillomavirus(HPV) is the most common sexually transmitted disease in the United States. The Centers for Disease Control estimates approximately 10% of men and 3.6% of women have oral HPV. It can infect the mouth and throat and cause squamous cell carcinoma, known as oropharyngeal cancer (OPC), including on the base of the tongue and the tonsils. Seventy percent of OPC in the United States is caused by HPV. Alcohol and tobacco products may also contribute to OPC.1
Patients with oral HPV are primarily asymptomatic; screening for the presence of the virus is an effective tool. When patients test positive for HPV, they should be referred to ENT doctors for examination and follow-up. This screening process can lead to early detection and removal of premalignant lesions, which would significantly reduce the risk of progression into cancer.
(this article originally appeared on page 74
of the Nov./Dec. 2022 issue of Dentistry Today)
ORAL HEALTH AND OVERALL WELL-BEING
The Global Burden of Disease Study 2019 states that oral diseases are estimated to affect nearly 3.5 billion people worldwide. According to the International Agency for Research on Cancer, lip and oral cavity cancers are among the top 20 most common cancers worldwide, with nearly 180,000 deaths yearly.
Oral HPV infection is ranked highly among oral diseases impacting overall health. The oral cavity serves as a source of early detection of medical conditions. Recent trends highlight the connection between oral and general health, which should not be ignored. This includes diabetes, endocarditis, and pregnancy.2 Dental practices can be active in patients’ overall well-being.
Routine dental visits can provide the optimal opportunity for oral HPV testing. Oral HPV testing follows the same approach used in the past for cervical cancer screening. The incidence of cervical cancer was rising until cervical Pap smear screening programs were implemented. High-risk HPV PCR testing became an essential component of the screening because of the sensitive nature of the test and its ability to detect changes at the molecular level that precede morphological abnormalities.
HOW ARE THE SAMPLES COLLECTED?
The oral HPV test kit includes a swab and a tube containing viral transport media. The dentist or dental hygienist performs the swab of the oropharynx, places the swab in the tube, and sends it to the laboratory. The cost to the patient is reasonable. The benefits far outweigh the cost.
ORAL CANCER IN YOUR PRACTICE
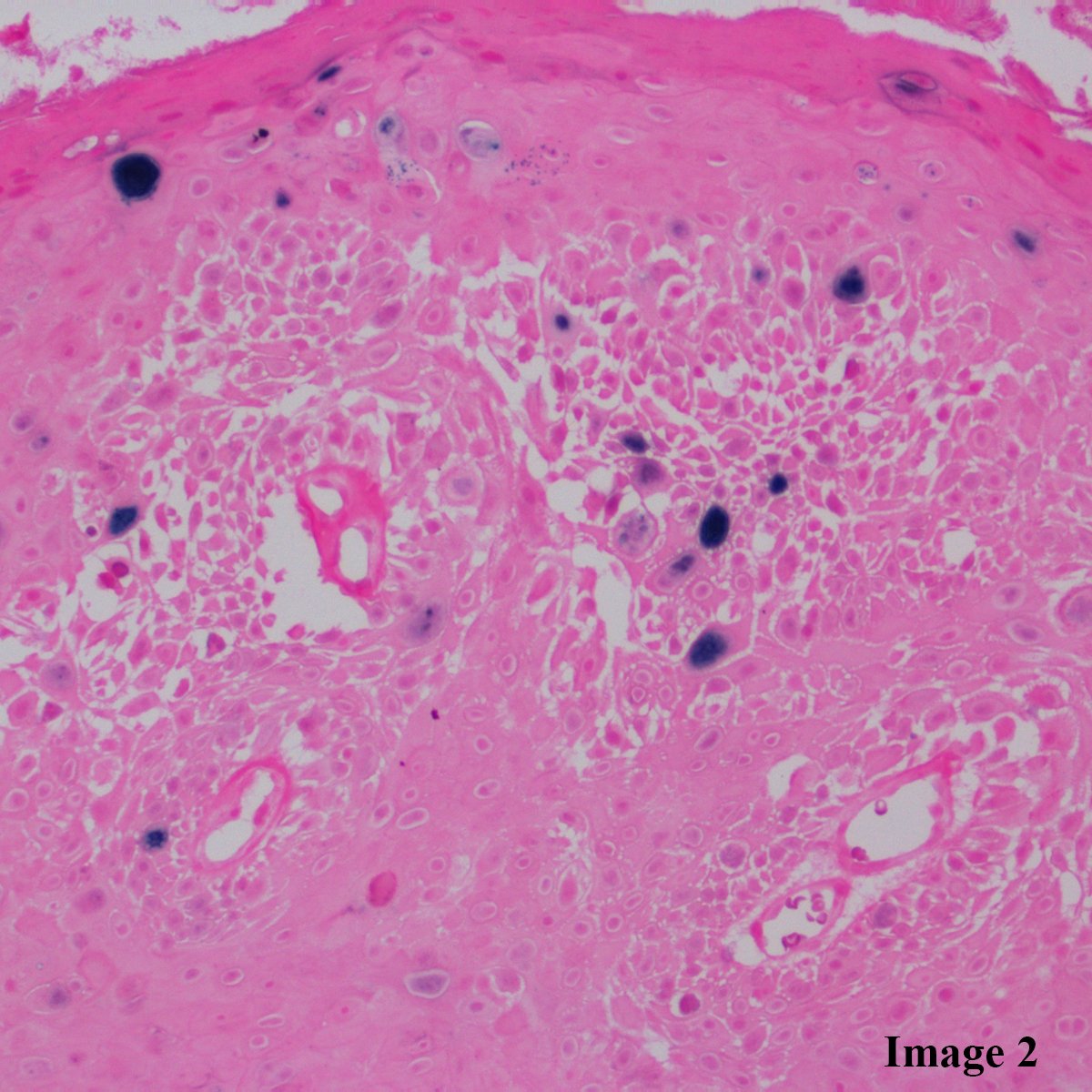
When suspicious oral lesions are biopsied, the pathology laboratory can perform histologic examination of the tissue and use ancillary testing for HPV subtyping to look for low- and high-risk HPV strains.3 Furthermore, testing for p16, a surrogate marker for oncogenic HPV, is becoming a standard practice to help detect high-grade squamous dysplasia and identify HPV-associated carcinoma. When we implement oral HPV screening, we identify high-risk patients at the earliest possible opportunity.
CONCLUSION
More than 100 types of HPV are divided into lowrisk (LR) and high-risk (HR). Testing for HR-HPV is done using PCR technology to detect the 14 most common genotypes known to cause cancer.
In modern dentistry, the dentist is essential in educating patients about various risk factors and lifestyle activities that impact their overall health. When patients are informed and educated about oral HPV, the decision to take the test is more readily accepted.
In our healthcare system, there are numerous examples of missed opportunities to achieve early detection of serious conditions. Oral HPV testing will identify patients at risk for oral cancer.
For more information, visit OmniPathology Laboratory’s website at omnipathology.com.
References
1. Centers for Disease Control and Prevention. HPV and Oropharengeal Cancer. https://www.cdc.gov/cancer/hpv/basic_info/hpv_oropharyngeal.htm
2. Institute of Medicine (US) Board on Health Care Services. The U.S. Oral Health Workforce in the Coming Decade: Workshop Summary. Washington (DC): National Academies Press (US); 2009. 2, The Connection Between Oral Health and Overall Health and Well-Being. https://www.ncbi.nlm.nih.gov/books/NBK219661/
3. Kim SM. Human papilloma virus in oral cancer. J Korean Assoc Oral Maxillofac Surg. 2016;42(6):327-336. doi:10.5125/jkaoms.2016.42.6.327
Dr. Kamal is the CEO of OmniPathology Laboratory in Pasadena, Calif. He completed his pathology residency and fellowship training at UCLA.