CASE STUDY #4
Clinical History:
71-year-old male presenting with a floor of the mouth mass. Biopsies were obtained.
H&E
Histologic Findings:
Microscopic examination shows papillomatous growth of highly atypical squamous cells with marked nuclear pleomorphism, increased nuclear/cytoplasmic ratio and high mitotic activity reaching the top layers of the squamous epithelium. Many cells show koilocytosis (HPV change). The lesion was transected at the base. HPV subtyping by In-Situ Hybridization (ISH) was performed showing positive staining with high-risk HPV 16/18. Staining for low-risk probe HPV 6/11 was negative. Immunohistochemical staining for P16 shows diffuse strong positive pattern.
Diagnosis:
At least high-grade squamous dysplasia; cannot rule out invasion.
Discussion:
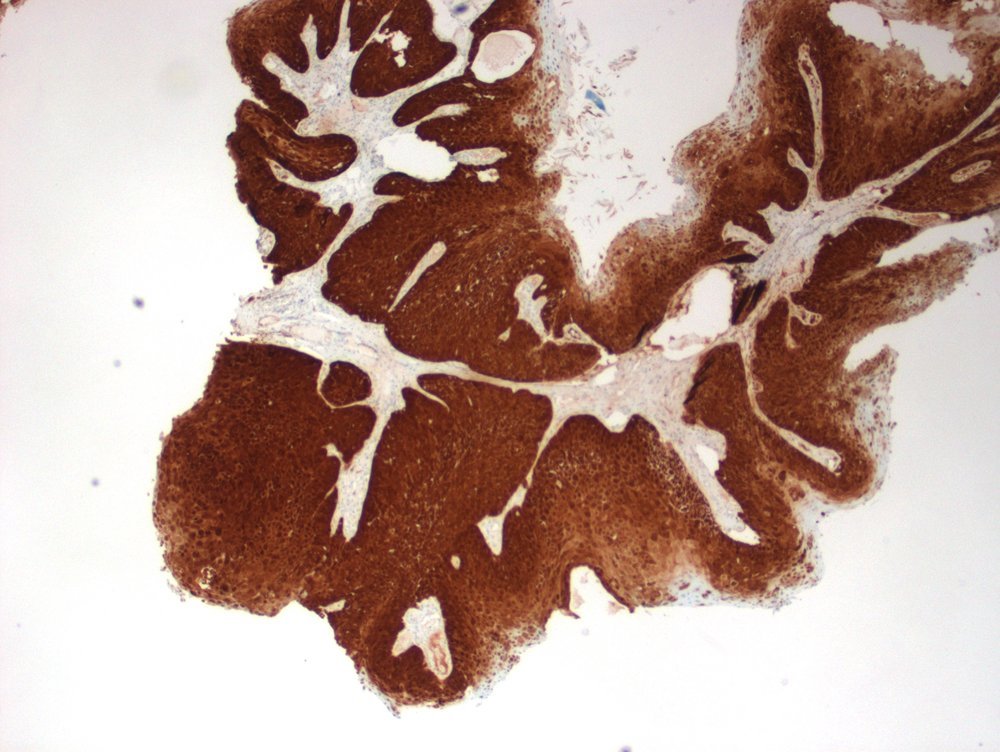
Image 3 P16-IHC
HIGH-RISK HPV 16/18
The morphological changes seen in this case represent malignant transformation of the squamous cells lining the floor of the mouth caused by Human Papilloma Virus (HPV). The diagnosis of high-grade dysplasia is made when the pathologist identifies highly atypical (abnormal) cells involving the full thickness of the oral mucosal lining with increased mitotic activity reaching the surface (Image 1). To confirm the link to HPV subtyping by ISH is performed on the biopsy tissue. There are many strains of HPV ranging from low-risk (LR) 6/11 to high-risk (HR) 16/18. In this case, the cells were positive for high-risk HPV 16/18 (Image 2). P16 is commonly considered a surrogate marker for oncogenic HPV infection. Image 3 shows diffuse positive staining pattern, supporting HPV associated high-grade dysplasia.
This case is an excellent example of HPV related oral cancer, a condition that can be detected at a much earlier stage if screening and early diagnosis of HPV were achieved.
Conclusion:
P16-IHC
HPV is the most common sexually transmitted disease in the United States. According to the CDC about 10% of men and 3.6% of women have oral HPV. HPV can infect the mouth and throat and cause cancers of the oropharynx (back of the throat, including the base of the tongue and tonsils). This is called oropharyngeal cancer. HPV is thought to cause 70% of oropharyngeal cancers in the United States. Alcohol and tobacco products may also contribute to oropharyngeal cancer. Since patients with Oral HPV may be asymptomatic, screening for the presence of the virus would be an effective tool to follow up HPV positive patients and detect early premalignant lesions, which would significantly reduce the risk of progression into cancer.
References:
1- https://www.cdc.gov/cancer/hpv/basic_info/hpv_oropharyngeal.htm
2- Sathish N, Wang X, Yuan Y. Human Papillomavirus (HPV)-associated Oral Cancers and Treatment Strategies. J Dent Res. 2014;93(7 Suppl):29S-36S. doi:10.1177/0022034514527969
3- Kim SM. Human papilloma virus in oral cancer. J Korean Assoc Oral Maxillofac Surg. 2016;42(6):327-336. doi:10.5125/jkaoms.2016.42.6.327
4- Chung CH, Gillison ML. Human papillomavirus in head and neck cancer: its role in pathogenesis and clinical implications. Clin Cancer Res. 2009 Nov 15;15(22):6758-62. doi: 10.1158/1078-0432.CCR-09-0784. Epub 2009 Oct 27. PMID: 19861444.