CASE STUDY #1
CLINICAL PRESENTATION:
An 83-year-old female presented for screening colonoscopy. The endoscopic findings included the presence of patchy erythema and erosions in the ascending colon and otherwise normal colon. No evidence of cancer, diverticulosis, colitis or AVM noted in the whole colon. The clinical information provided by the gastroenterologist also included history of liver cirrhosis with signs of portal hypertension noted.
HISTOLOGICAL FINDINGS:
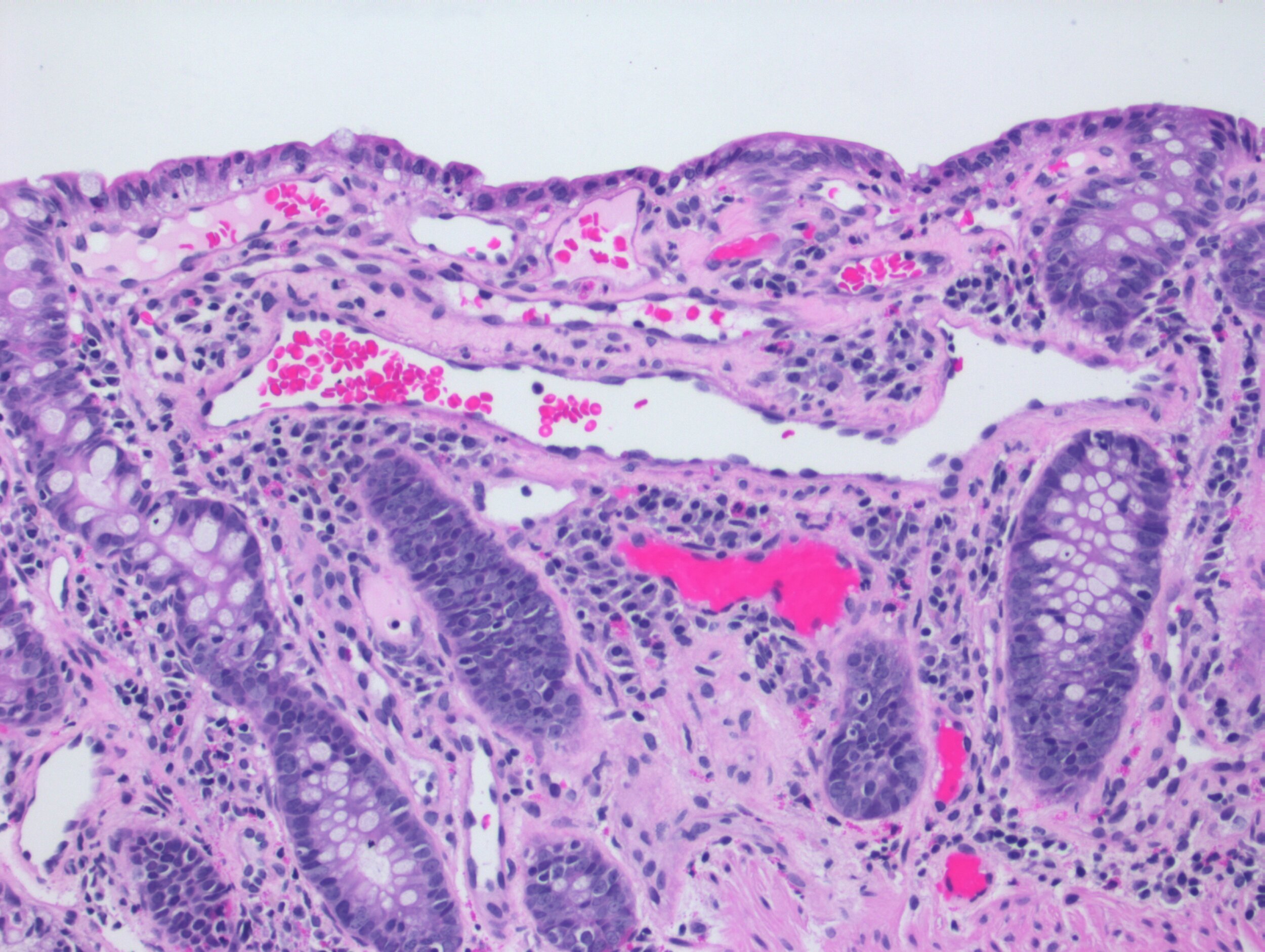
Biopsies of the ascending colon show mildly distorted architecture and increased number of the lamina propria capillaries with vascular ectasia and branching as shown in the attached photomicrograph.
DIAGNOSIS:
Portal Hypertensive Colopathy (PHC)
DISCUSSION:
PHC is a vascular abnormality that can be seen in any part of the colon. Endoscopically, it presents as erythematous lesions. The main complication of PHC is lower GI bleeding. In our practice, when we encounter prominent dilated vascular structures in colonic biopsies, the top entities we consider in the differential diagnosis are vascular ectasia (originally called angiodysplasia), radiation colitis and portal hypertensive colopathy. Vascular ectasia (angiodysplasia) are considered vascular malformation commonly seen in older populations. Radiation colitis is usually associated with mucosal vascular dilatation surrounded by stromal fibrosis and, in some cases, endothelial and epithelial abnormalities. Epithelial atypia and cytomegaly without increase in the N/C ratio can also be seen in radiation colitis. History of radiation treatment is required to make this diagnosis. Portal hypertensive colopathy is seen in cases of portal hypertension due to liver cirrhosis.
According to the study by Ito et. Al, histologic examination of 47 cases of cirrhotic patients showed the histologic evidence of PHC in 31 cases (66%). In this study 23% were seen in the rectosigmoid, 11% in the descending, 24% in the transverse colon, 23% in the ascending colon and 16% in the cecum.
CONCLUSION:
The presence of vascular ectasia in colonic mucosal biopsies is a nonspecific finding. However, with good clinical history, a more definitive diagnosis can be made, as in this case. Systematic approach to mucosal biopsies helps in identifying subtle morphological changes. In the case of radiation colitis, the history of radiation treatment may be remote, therefore not listed on the requisition. Considering the possibility, contacting the submitting physician and inquiring about history of malignancy and radiation therapy can be extremely useful.
REFERENCE:
Ito K, Shiraki K, Sakai T, Yoshimura H, Nakano T. Portal hypertensive colopathy in patients with liver cirrhosis. World J Gastroenterol. 2005;11(20):3127–3130. doi:10.3748/wjg.v11.i20.3127
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4305852/pdf/WJG-11-3127.pdfLewin, Weinstein and Riddlle’s Gastrointestinal Pathology and its Clinical Implications, Riddlle and Jain, Second Edition, Wolter Kluwer Health